a
MEDICAL COMMUNICATIONS
company
Empowering clinicians.
Making a difference in the lives of patients.

Loading 01%
a
company
Empowering clinicians.
Making a difference in the lives of patients.
a MEDICAL COMMUNICATIONS company
As a true partner, we immerse ourselves in our clients' strategy and imperatives so that we are able to make the most meaningful and thoughtful recommendations for tactical execution. We utilize advanced data and analytics to ensure desired outcomes are delivered.
a STRATEGIC PLANNING company
Building and executing on your brand objectives and imperatives
More
than
45
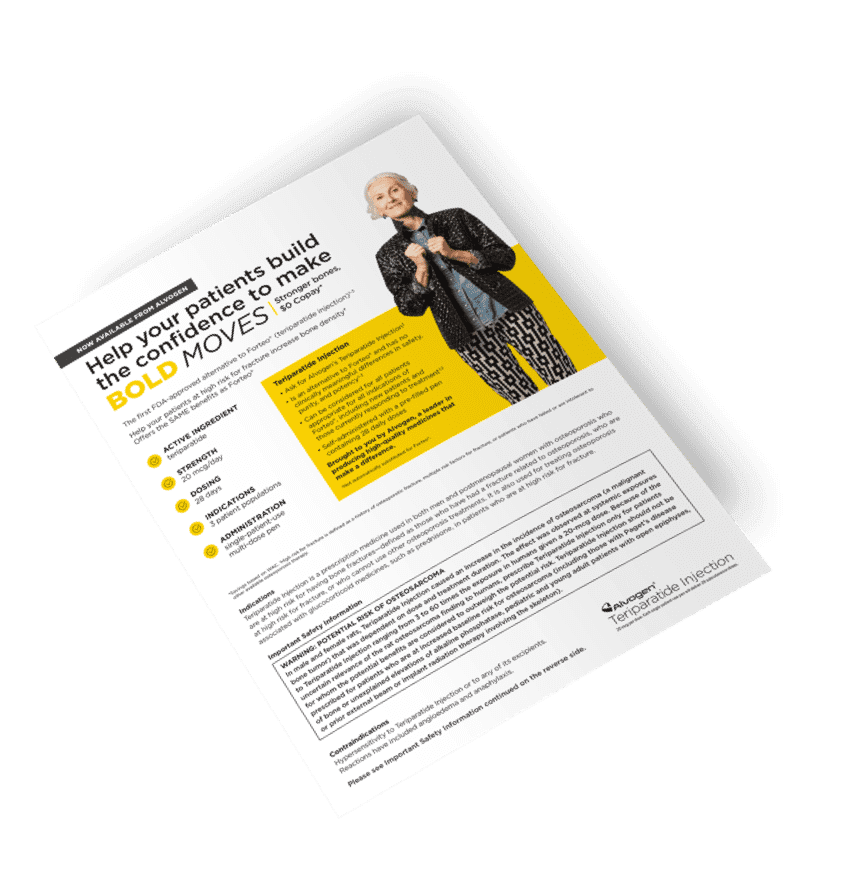
a CONTENT DEVELOPMENT company
Translating your scientific advances
More
than
20
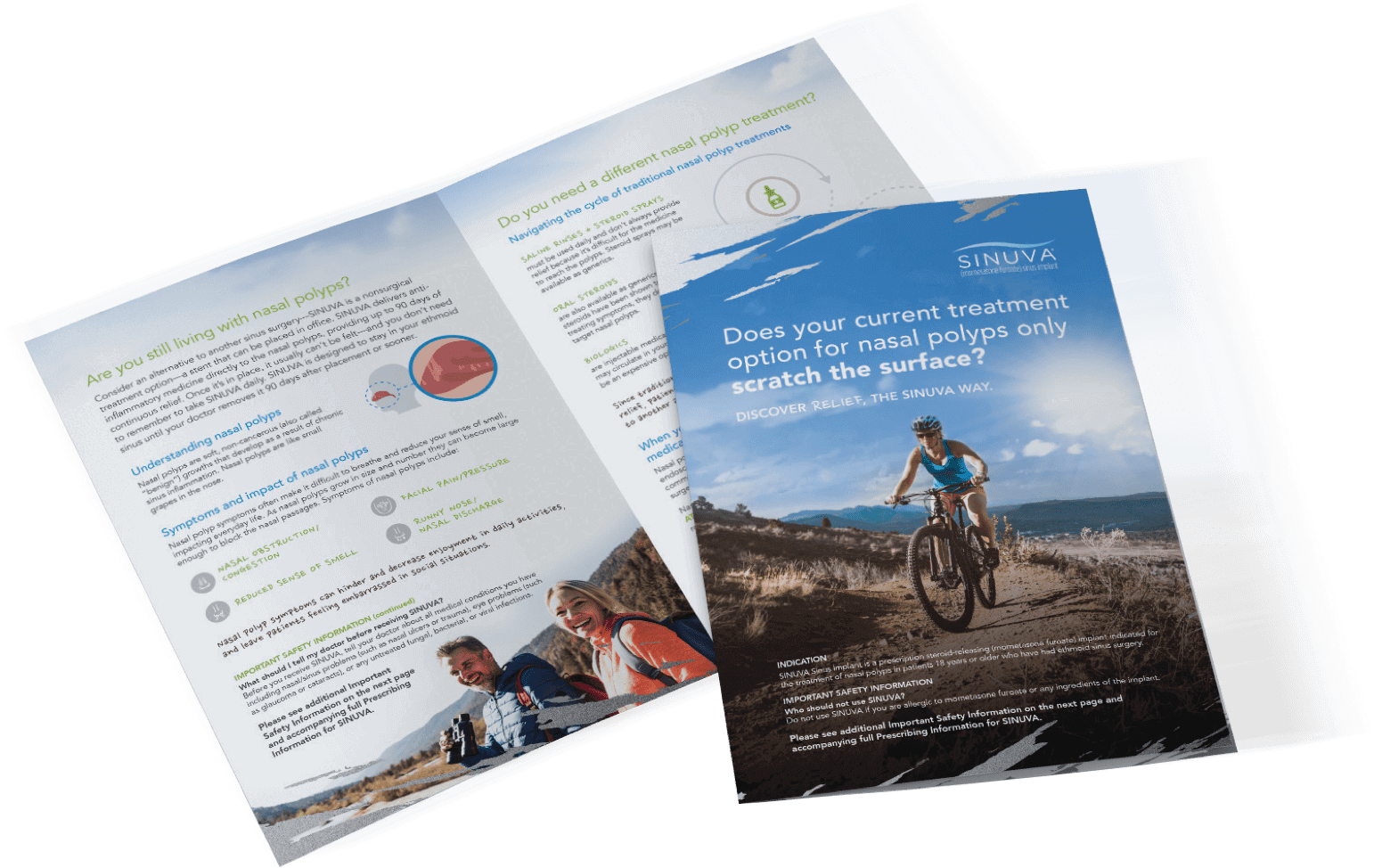
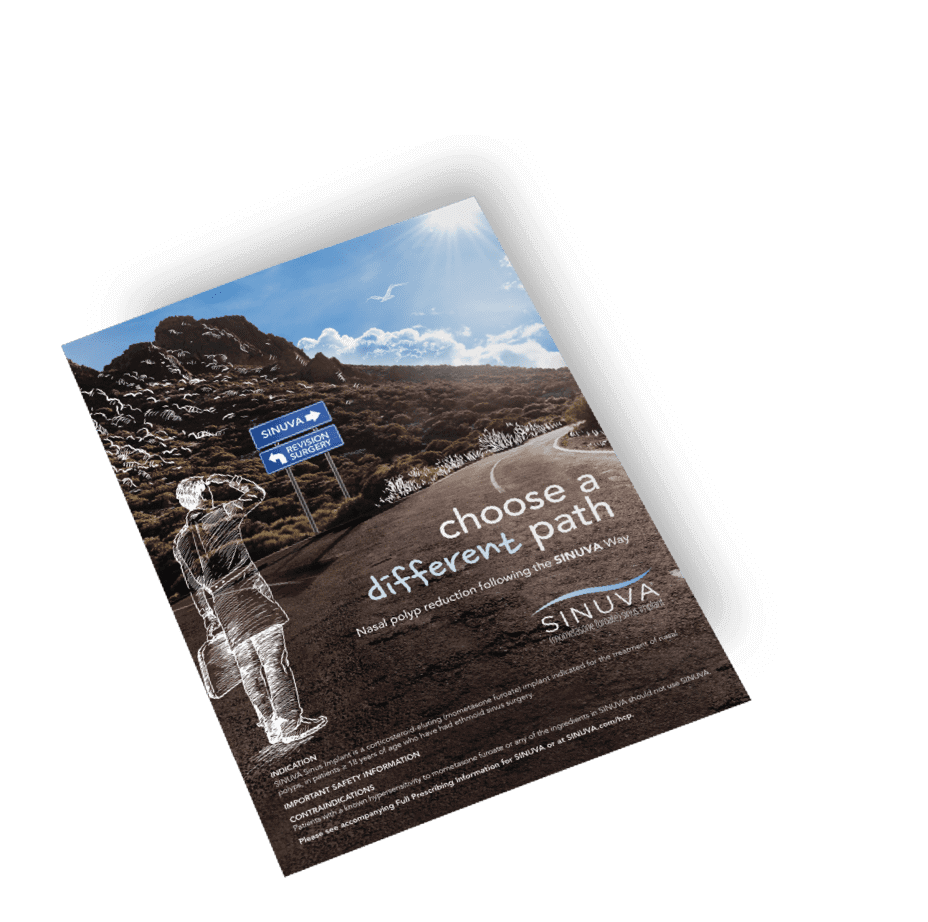

a CREATIVE company
Bringing Art
to the Science
a PERSONALIZED MARKETING company
Providing critical insights and
predictive modeling
Behavioral
data from
2
Million
HCP Profiles
a DIGITAL company
Working “behind the screens” to develop meaningful interactions by asking and answering essential questions
3-5 Minutes
Average engagement with brand message
Flawless execution of personal HCP engagements
Facilitate
over
120
a LIVE MEETINGS company
Flawless execution of personal HCP engagements
Facilitate
over
120
Going Virtual?
We've got you covered.
Learn More
a DATA & ANALYTICS company
Providing critical insights and
predictive modeling
2:1
Average
Proven ROI
a CONTENT MARKETING company
Prescribing Alert Launch Kit
Launching your brand successfully
is mission critical to your business.
PRI is expert at delivering:

a GRATEFUL company
a TALENTED company
a CONNECTED company
Our clients enjoy the strategic advantage that comes from our connection to Haymarket’s growing family of medical brands
More
than
70
a DYNAMICALLY GROWING company
JOIN OUR TEAM!
Our philosophy is quite simple: only by having the highest quality individuals can you produce the highest quality products, combining the best in content, design, technology, and client services.
1 / 1
an EASY-TO-REACH company
PRI Healthcare Solutions
A division of Haymarket Media
1-201-799-2500