








What Is Pulmonary Arterial Hypertension?
Pulmonary arterial hypertension (PAH) is a rare subset of pulmonary

*CTEPH=chronic thromboembolic pulmonary hypertension

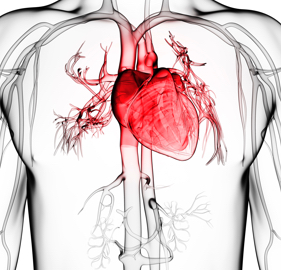
PAH affects the blood vessels of the heart and lungs and is defined by its hemodynamic criteria, shown
In PAH, progressive increase in pulmonary vascular resistance (PVR) of > 3 Wood Units (WU) is accompanied
by right heart dysfunction, which ultimately leads to right-sided heart

Normal
The resting mPAP is 14 ±

PAH
The PVR and pulmonary pressures are higher than normal due to obstructed or narrowed pulmonary arteries
caused by endothelial dysfunction and vascular

PAH is defined by2-4*
mPAP=mean arterial pulmonary arterial pressure; PAWP=pulmonary arterial wedge pressure; PVR=pulmonary vascular resistance.
*All values measured at rest.


PAH is a rare disease and affects 15 to ~52 people per million patients, in countries where studies have
been
*These studies were: the French Registry data from France based on 674 PAH cases from 2002-2003, estimating a prevalence of 15 cases/1 million per population and the hospitalization data from the Scottish Morbidity Record, which was based on 374 cases from 1986-2001 giving a prevalence of 52 cases per million population.


The average age of a newly diagnosed patient has dramatically changed since the 1980s.
†Data are from both the Patient Registry for the Characterization of Primary Pulmonary Hypertension and the Registry to Evaluate Early and Long-term PAH disease management (REVEAL Registry). The Patient Registry for the Characterization of Primary Pulmonary Hypertension, initiated by the National Institute of Health in 1981. This multicenter, prospective registry included 32 medical centers in the United States with 187 patients with primary pulmonary hypertension enrolled from July 1981 to September 1985. Limitations include lack of standardized follow-up assessments; prospective studies are needed to validate findings. The Registry to Evaluate Early and Long-term PAH disease management (REVEAL Registry), a large, multicenter, prospective cohort registry that included 54 centers in the United States. 2,967 patients were enrolled between March 2006 and September 2007, all with newly or previously diagnosed World Health Organization group I PAH and pre-specified hemodynamic criteria by right-heart catheterization test. Limitations include lack of standardized follow-up assessments; prospective studies are needed to validate findings.

Approximately 80% of PAH cases are seen in
Nationally, approximately
2.8 years
is the mean time from symptom onset to PAH diagnosis, according to the REVEAL Registry. Most patients are
in NYHA FC III at the time of


Patients with PAH typically present with non-descript symptoms that mimic those of other more common
disease


Since PAH is a diagnosis of exclusion, many tests are required to assess the probability of this





According to the
2015 European Society of
Cardiology/European Respiratory Society (ESC/ERS) Guidelines, echocardiography should always
be performed when PH is suspected and may be used to infer a diagnosis of PH in patients with multiple
different echocardiographic measurements consistent with this


RHC is the only definitive procedure to confirm PAH and is recommended for all adult patients with
The formal diagnosis of PAH is based on the following results from the RHC test.
Elevated mean pulmonary arterial pressure (mPAP):
Normal pulmonary artery wedge pressure (PAWP):
Elevated pulmonary vascular resistance (PVR): >3 Wood Units (WU)
*All values are measured at rest.


It is imperative to assess the patient's functional classification (FC) to help establish disease
severity. WHO classifies patients according to their FC from I to IV (see table
Class | Symptoms
Patients with PH in whom there is no limitation of usual physical activity; ordinary physical activity does not cause increased dyspnea, fatigue, chest pain, or presyncope
Patients with PH who have mild limitation of physical activity. There is no discomfort at rest, but normal physical activity causes increased dyspnea, fatigue, chest pain, or presyncope
Patients with PH who have a marked limitation of physical activity. There is no discomfort at rest, but less than ordinary activity causes increased dyspnea, fatigue, chest pain, or presyncope
Patients with PH who are unable to perform any physical activity at rest and who may have signs of right ventricular failure. Dyspnea and/or fatigue may be present at rest, and symptoms are increased by almost any physical activity
Monitoring FC is important when developing a plan for the treatment and
changes in the patient’s


The 6-minute walk test (6MWT) helps to address the severity of disease progression as an overall
indicator of functional


As recommended in recent ESC/ERS guidelines, the overall goal of therapy should be achievement of a low
risk
Currently, multiple therapies for PAH are approved by the Food and Drug
Administration (FDA) that fall into 3 therapeutic
Prostacyclin pathway
Endothelin pathway
Nitric oxide pathway
The
2015 ESC/ERS Guidelines
recommend following the PAH management algorithm when deciding therapy goals and treatment



Nurses are an essential part of the health care professional team in the journey of a patient with PAH.
Roles include19:


The 2015 ESC/ERS guidelines recommend that the PAH team collaborates with other professionals, including
psychologists, psychiatrists, social workers, and
patient
A multidisciplinary environment can be provided in large-volume expert


Patients may differ in their preferred way of learning; therefore, communicating information needs to
match the individual's


Beginning the discussion of PAH with patients can be emotional and overwhelming for the patient as there are many questions the patient may have when they are diagnosed.
Teaching should include the
The nurse can educate the
Awareness of a patient’s health literacy is an integral component in patient care, safety, education, and


The diagnosis of PAH can be devastating to a patient, as many aspects of their daily life may be affected.
Patients with PAH

In female patients with PAH that may become pregnant, a discussion regarding pregnancy and their disease is necessary.


Since PAH is a progressive disease without a cure, end-of-life and ethical issues may need to be addressed.
How Does the Patient Receive Optimal Treatment?
Patients who are involved in the decision making regarding their disease are more engaged
and


Patient activation or patient engagement, is just one aspect of an individual’s ability to engage in
their own
Patient must believe that their role is important in managing their own health
Having the confidence and knowledge necessary to take action
Patient takes action to maintain and improve their health
Patient continues with self-management, even under stress

Further challenges arise when some patients may not wish to be engaged in the management of their


It is important to educate the patient both on the medications they have been placed on and the importance of filling prescriptions and adhering to the scheduled doses.


Patients should be counseled on their own physical care to prevent potential harmful situations.


Caregivers play a key role in supporting patients with PAH in the management of their disease, along with
every day physical and emotional
Caregivers benefit from receiving appropriate


Patients with PAH have a progressive condition which can cause them to have anxiety and/or
Support groups can offer short- or long-term support to help patients manage anxiety or
Psychosocial patient support should
Patients increasingly seek information regarding PAH via the
This MPR/PulmonologyAdvisor Fact Pack is produced as a basic reminder of important information for healthcare professionals. Readers are advised to consult manufacturers and specialists if questions arise about specific products, treatments, or diseases. The publisher and editors do not assume liability for any errors or omissions. MPR, PulmonologyAdvisor, and Fact Pack are registered trademarks of